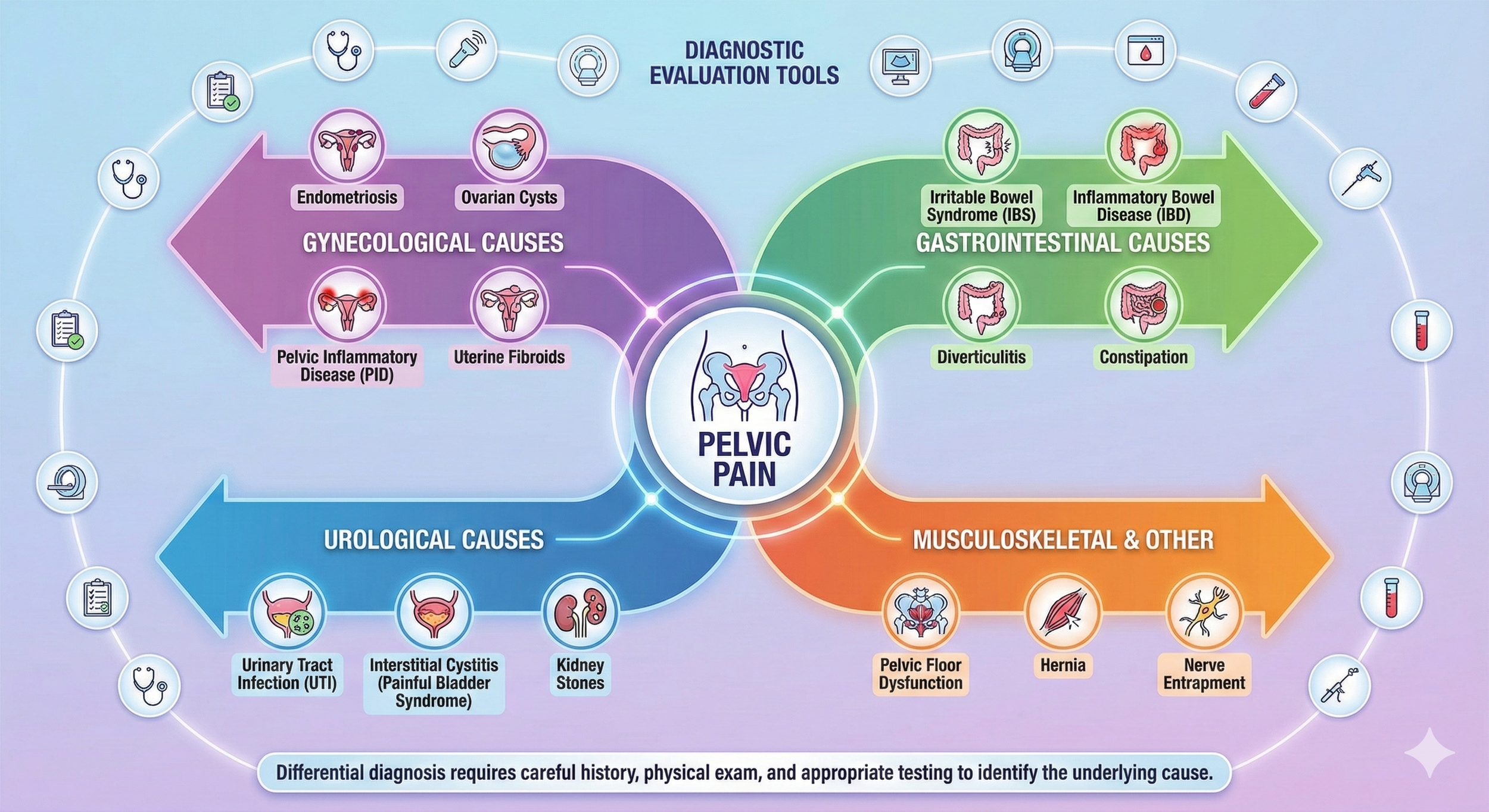
Gynecological Causes (Reproductive System)
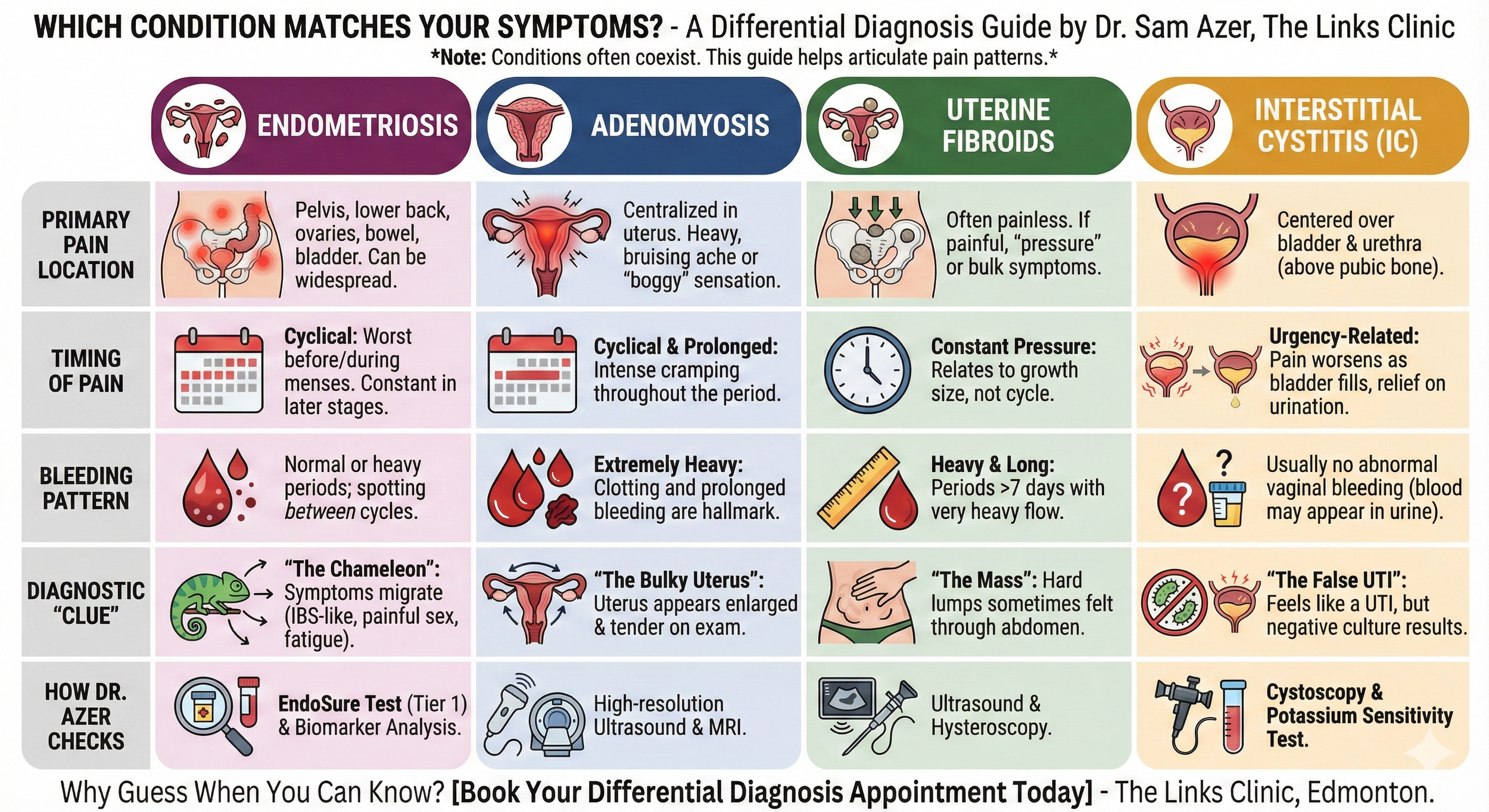
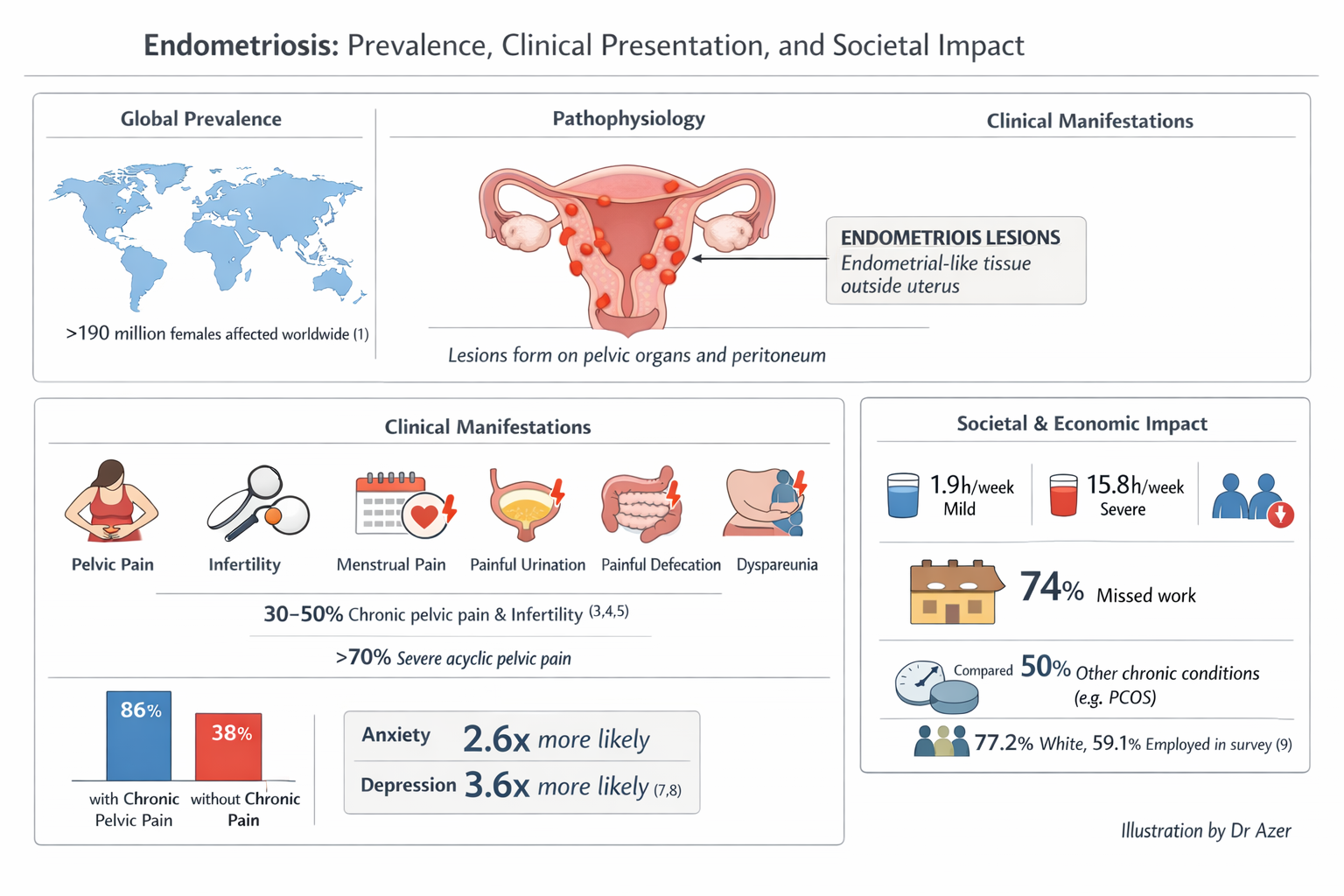
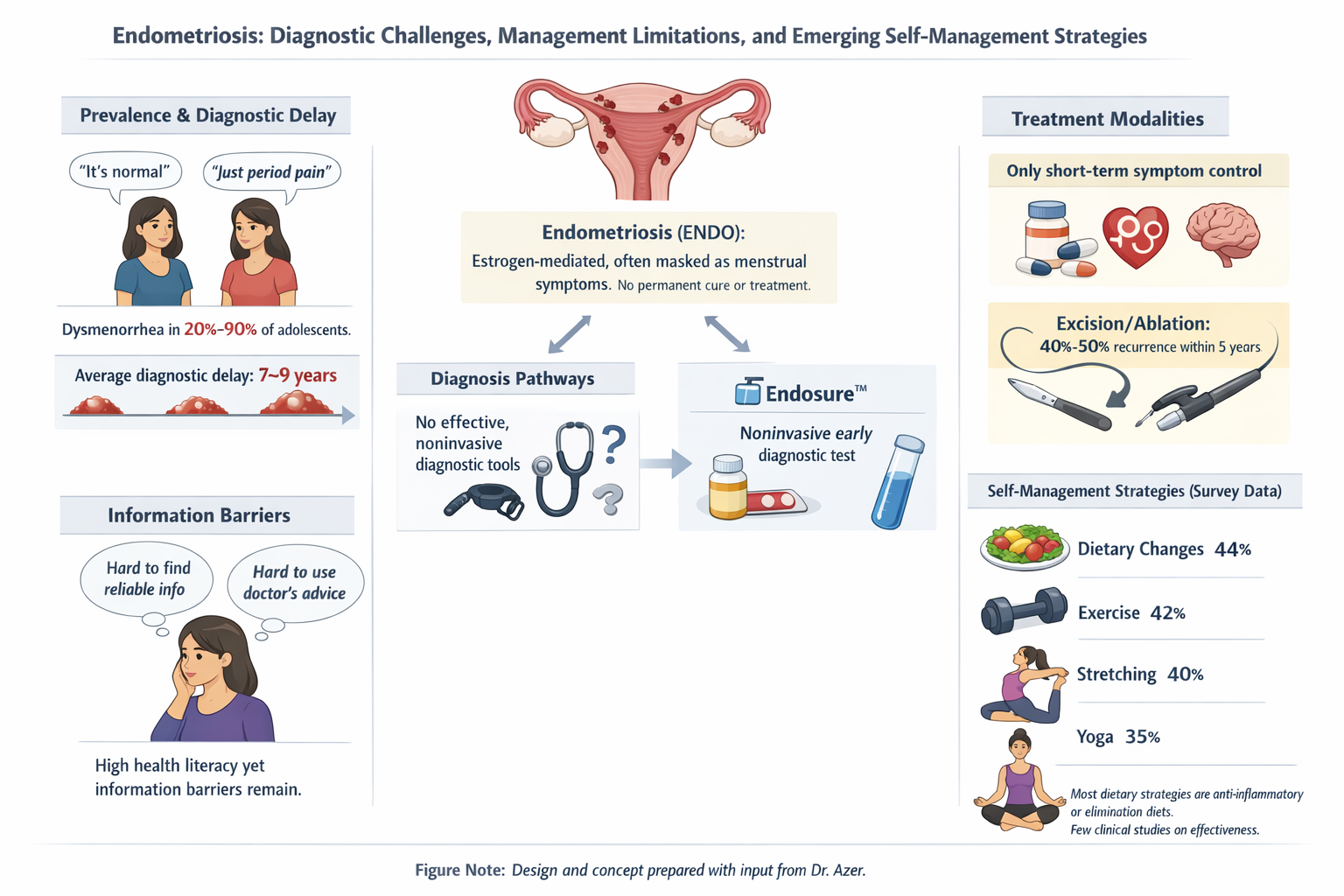
Endometriosis: Tissue similar to the uterine lining grows outside the uterus, causing inflammation, scarring, and chronic pain that can be cyclic or constant.2 This is the specific condition the Endosure test is designed to detect.3
Adenomyosis: Endometrial tissue grows into the muscular wall of the uterus, often causing heavy, painful periods and an enlarged uterus.4
Fibroids (Leiomyomas):5 Non-cancerous growths in or on the uterus that can cause pressure, heaviness, or sharp pain if they press on nerves or organs.6
Pelvic Inflammatory Disease (PID): An infection of the reproductive organs, often resulting from STIs, which can lead to long-term scarring and pain.7
Ovarian Cysts: Fluid-filled sacs on the ovaries that can cause sharp pain if they rupture, bleed, or twist (torsion).8
Pelvic Congestion Syndrome: Enlarged, varicose-type veins around the uterus and ovaries that cause dull, aching pain, often worse when standing.9
Pelvic Adhesions: Bands of scar tissue from previous surgeries, infections, or endometriosis that bind organs together, causing pulling or sharp pain.10
Non-Gynecological Causes
Urinary Issues: Conditions like Interstitial Cystitis (painful bladder syndrome), urinary tract infections (UTIs), or kidney stones can cause significant pelvic discomfort.11
Gastrointestinal Issues: Irritable Bowel Syndrome (IBS), constipation, diverticulitis, or inflammatory bowel disease (IBD) often present with pelvic pain and bloating.12
Musculoskeletal Problems: Tension in the pelvic floor muscles (high-tone pelvic floor), hernias, or nerve entrapment (like pudendal neuralgia) can cause chronic pain.13
Psychological Factors: A history of trauma or abuse, as well as chronic stress or depression, can be linked to or exacerbate chronic pelvic pain.14
"Diagram showing common locations of endometriosis lesions and adhesions in the pelvis."